Warning: This post has some gnarlier-than-average pictures, if you're squeamish, proceed with caution.
There are always a couple of more memorable individuals I have the privilege of knowing for their brief time on board. I get a tiny glimpse into their lives, and they probably won't remember me a few months from now, but they have captured a piece of my heart, and I won't be forgetting them anytime soon.
A Noma Life
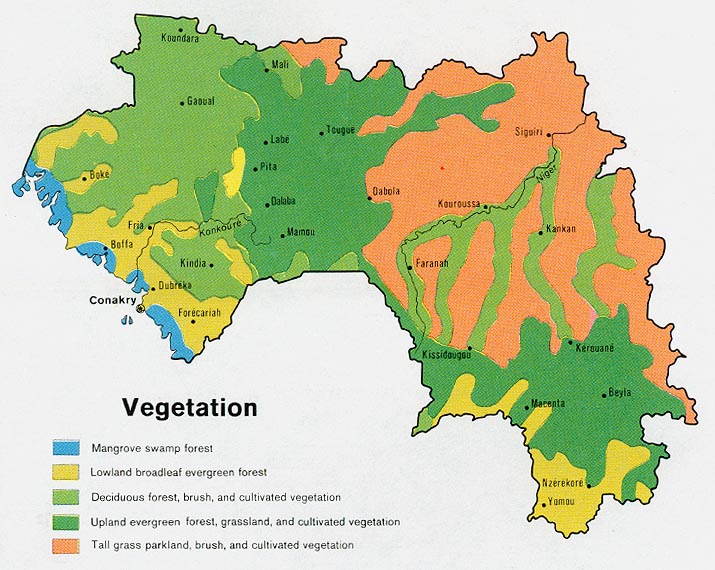
As a child, Aicha was afflicted by a disease called Noma.
Noma is one of those diseases that is essentially non-existent in developing countries, where sanitation, decent nutrition, and dental care are just the norm. It usually effects children in the poorest countries in the world, and has a 90% mortality rate. Bacterial infection in the oral mucosa leads to a painless, but incredibly fast necrosis (death) of the surrounding tissue. In short, this disease eats your face off, sometimes in a matter of days. If treated quickly with antibiotics, it can be stopped, but the lost tissue will never grow back. The 10% who are lucky enough to survive this initial onslaught are horribly disfigured for life. This disease doesn't happen to the kind of people in the kind of places where reconstructive plastic surgery is an option. It also so happens, as is true of many of the conditions we treat on board, that such disfiguration is widely viewed in these parts as an outward sign of an inner evil. It is a scourge on all aspects of one's life.
 |
| Tahina, a patient with Noma I met in Madagascar. |
Flash back to 2009.
Aicha, then 5 years old, was living with her Fulfulde-speaking grandmother and uncle in the Extreme North region of Cameroon. Her father and mother had abandoned her. When she became infected with noma, her uncle brought her to the nearest hospital - a scarf wrapped around her face to hide the devastation. She was incredibly malnourished as well, and weighed only 24 pounds. The infection was treated and she received nasogastric feedings, saving her life, but she was left with a gaping hole where her right cheek used to be.

Hôpital de Meskine, where she was brought, is run by an American non-profit, and provides care regardless of the ability to pay. They knew the best plan for Aicha was specialized surgical care, but they are only equipped for minor surgical procedures. One of the surgeons volunteering at this hospital happened to have worked here on the ship a few times in the past, and knew Dr. Gary Parker, our resident expert in these matters. The next field service for the Africa Mercy was planned for Lomé, Togo; some 1,500 km and two countries away. Although it was an incredibly long journey through Nigeria and Benin, the hospital team was able to arrange for Aicha to come to Togo and receive reconstructive surgery from some of the top surgeons in this rather niche specialty.
 |
| Aicha in 2010 |
Fast forward to a few weeks ago. A slender, bubbly, cropped haired teenager is grabbing my arm, pulling me from the corridor into D Ward. "Tantie! Tantie Haousa!" (Auntie Haousa - the nickname she gave me). "Travaille ici aujourd'hui?" In my broken french, I explain no, I'm not working today. I'm working in the office instead. But I promise to pop my head in every time I pass by. She shakes her head, a mischievous grin on her face. "Non! Travaille ici!" I make note of her nail polish - she would remove & repaint them 2 or 3 times a day. "Désolé, ma copain." Not today. We hug, and I linger, cherishing the moment. There's always one patient; one I don't want to let go of.
 |
| Aicha a few weeks ago |
Later that day, as I passed the ward again on my way to lunch, I see her gazing at the TV while another patient ties her very short hair into many tight bunches. She's preoccupied. I'll come back after lunch.
She was discharged while I was eating lunch. I never really got to say goodbye.
A selfish thought, of course. She loved *all* the nurses, and all of us loved her; I'm sure she had a lovely send-off. Perhaps, as well, it's better off this way. Easier to move forward, not looking back. The more time patients spend on the ship, the harder it can be for them to leave this bubble and return to the real world.
-
A couple days later I was sorting through piles of patient charts, ordering all the pages before they are to be scanned for our digital archive. I came across hers, and, for the first time saw the above pictures of her from 8 years ago. I was never actually assigned to her; had never looked in her chart. I couldn't believe those somber, apprehensive eyes could possibly be the same girl.
After her visit to the AFM in 2010, Aicha left the ship looking like a whole different person - and not just because of the reconstruction. Her face was whole again, but her eyes had a twinkle that was a lot more familiar to me.
Her eye, as it happens, was the reason Aicha came back to the ship here in her home country, 8 years later. You can kind of see it on the photos above, even before the repair. Her right eye sags a bit, pulled down by the tight scar tissue below. The graft healed quite nicely for her; though it is darker than the rest of her face, it is still pretty good lookin' compared to the alternative. As a young woman, she now holds her head high, obviously confident in her natural beauty and radiant personality. As her graft had healed and the swelling dissipated, however, the skin below her eye was pulled further down, making it difficult to close or blink.
The solution was a relatively simple procedure this time around, and it's easy to see that this girl is gonna go places. She is fluent in French now, excelling in school, and just so darn charismatic it hurts. I had a good little cry that night I knew I'd probably never hear "Tantie Haousa" again, and another good little cry writing this post. I can only hope and pray that this tenacious soul continues to defy the odds, and that she continues to bring joy and laughter into the lives of those around her.
 |
| Aicha (right) with nurse Alex & baby Mas-Oudatou (cleft palate patient) |
Love you, Aicha.
À la prochaine,
-D
Update: BBC's Pidgin division produced a news story on the Ship's service here in Cameroon, and you might catch a glimpse of Aicha teaching me and another nurse a clapping game: